Brain Transplant: Is It Feasible?

Dan Baumgardt, University of Bristol
The neurosurgeon Sergio Canavero announced in 2015 that he could soon be capable of performing the world’s first human head transplant procedure. This would mean that it would be possible to remove someone’s head, and graft it onto the neck and shoulders of another person. As of yet, this has only been performed on cadavers and not on living humans.
But suppose you want to keep the face that you’ve already got? Or have grown tired of the body you inhabit? Could it ever be possible to switch brains between bodies instead?
Emma Stone recently won her second Oscar for her performance in the brilliantly surreal comedy Poor Things. In the film, Stone’s character, Bella Baxter, receives a brain transplant from her surviving unborn child after killing herself. The surgery is performed by experimental scientist Dr Godwin Baxter (played by Willem Dafoe).
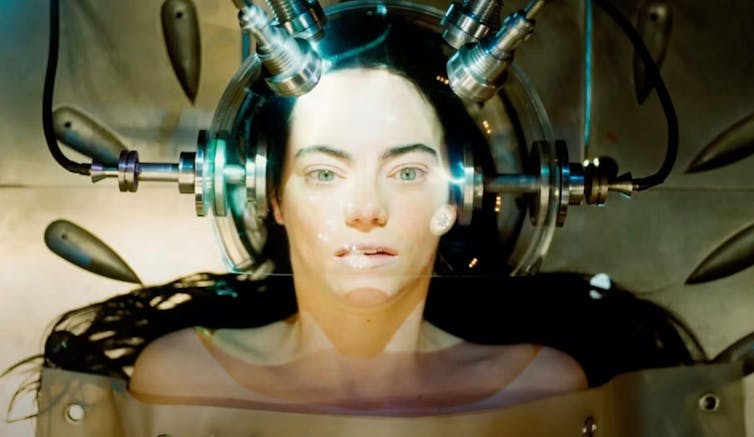
Anyone who’s watched the film will see Dr Baxter remove the brain from the back of the skull, shelling it as easily as a pea from a pod.
For reasons I’ll explain later, this scene isn’t anatomically correct, but it does beg the question – how feasible is it to perform a brain transplant? What are the practicalities in perhaps the most challenging operation ever conceived?
Challenge one: getting in, getting out
The living brain has the texture of soft-set blancmange, and is protected from harm by the skull. Despite being a tough nut to crack, the bone would probably prove the easiest structure to negotiate. Modern neurosurgical techniques make use of craniotomy saws to remove a patch of skull, and access the brain underneath.
It’s worth noting that not all neurosurgical operations reach the brain this way. The pea-sized pituitary gland sits upon the brain’s base, just behind one of the sinuses at the back of the nasal cavity. In this case, it makes sense to use the nose instead for pituitary surgery.
Although the nose wouldn’t be big enough to insert a new brain through, it can certainly act as a route for removing one – albeit in pieces. During the mummification process ancient Egyptians, who regarded the brain as unimportant, removed bits of it via the nasal passages.
Past the skull, you reach the swaddling of the brain – three protective membranes, or meninges. The first, the dura, is tough. The second, the aptly named arachnoid, is like a spider’s web, while pia, the third, is delicate and invisibly thin. It’s these structures that become inflamed in meningitis.
These membranes provide stability and prevent the brain from sloshing around. They also segregate the skull innards into compartments. The first provides a protective fluid cuff around the outside of the brain – think of gherkins floating in a jar of vinegar. Known as cerebrospinal fluid (CSF), it’s made from filtered blood and is colourless.
The meninges also make channels between brain and skull. These are the routes through which both blood and CSF from the head are returned back to the heart.
On opening up the skull and meninges, there will be enough of a window to remove the brain. This would prove the most straightforward part of the operation.
Challenge two: connecting up the circuits
Now it’s time to get the new brain in. This is where things get complicated.
The brain receives sensory information from all over the body and sends instructions back to it, making muscles contract, the heart beat and glands secrete hormones. Removing a brain requires cutting through the 12 pairs of cranial nerves which come directly off it, and the spinal cord. Information enters and exits the brain through all these structures. See the difficulty?
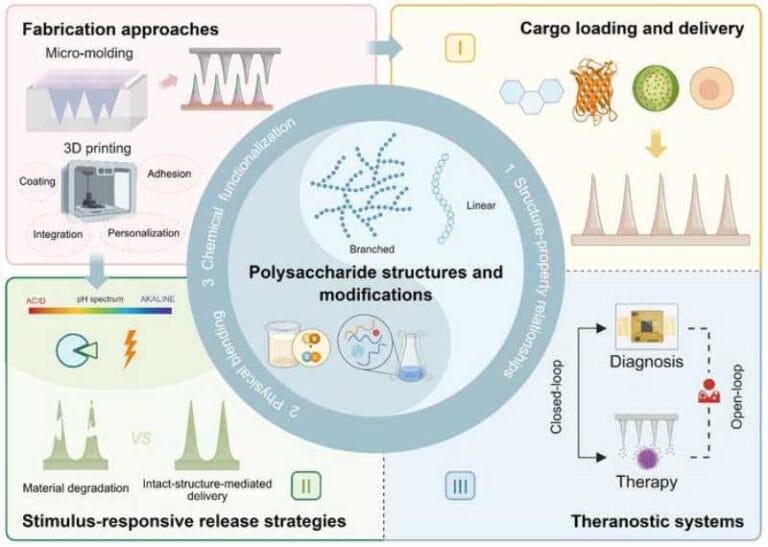
Nerves don’t simply join back together. As soon as you’ve cut them, they typically begin to disintegrate and die, though some are more resilient to damage than others. Research groups around the world experiment with how to promote regrowth of nerve cells after damage to avert neurological symptoms. Ideas about this might be achieved are manifold but include use of chemicals or grafting in cells that stimulate neuronal recovery.
Researchers have also suggested that a special biological glue could be used in order to stick two cut ends of a severed nerve or spinal cord back together.
Removing the old brain will have also required cutting through the arteries which provide blood. This will also have cut off critical oxygen and nutrition, which will also require recoupling.
Challenge three: the aftermath
The final, most uncertain period is the aftermath. And the list of speculations are endless. Will the subject regain consciousness? Will they be able to think? Move? Breathe? How will the body react to the new brain?
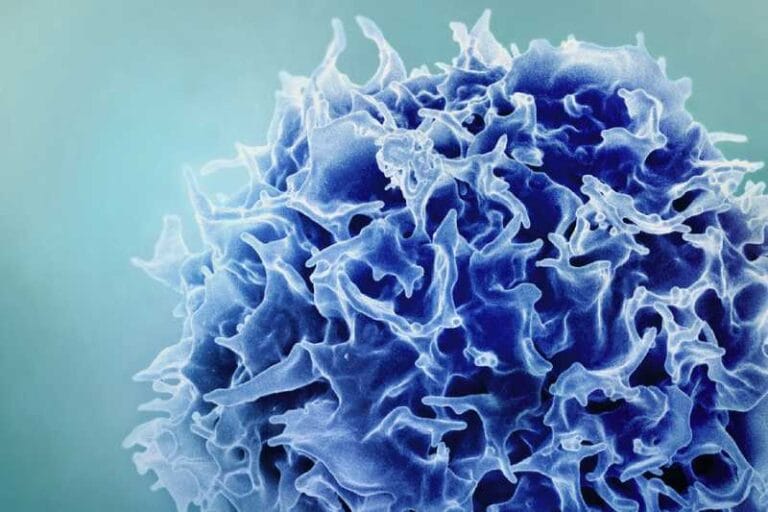
Most transplant surgeries require donors matched to recipients, since the body’s normal reaction to unknown tissues is to reject them. The immune system sends a cavalry of white blood cells and antibodies to attack and destroy, convinced this new presence means harm. Normally brains are protected from this onslaught by another shield, called the blood-brain barrier. If not properly reconstructed during the operation, the donor brain could be open to attack. https://www.youtube.com/embed/noa2SMWPn14?wmode=transparent&start=0
It’s equally important to consider how the brain will react to its new home. In Poor Things, Bella Baxter’s brain and body were reported to be “not quite synchronised”. But brains can learn to grow. So, just as babies gain an arsenal of thoughts, behaviours, skills and abilities during their childhood development, a transplanted brain might do the same.
So, brain transplantation currently remains the stuff of science fiction and academy award-winning cinema. Feasibility according to basic anatomy and physiology make developing such a complex procedure unlikely. But will more time, tools, technologies, expertise and, of course, money ever make it viable? If Poor Things offers a glimpse into the ethics of brain swapping, then that’s a frightening thought.
Dan Baumgardt, Senior Lecturer, School of Physiology, Pharmacology and Neuroscience, University of Bristol
This article is republished from The Conversation under a Creative Commons license. Read the original article.